A. For Abortion!

The Abortion Dictionary is a fortnightly blog series and is an attempt to dispel myths and provide safe and reliable information about safe abortion and attendant issues. We start with the basics and cover a range of topics from A-Z, quite literally! Happy reading!
Abortion
The word conjures up a myriad range of images, emotions, taboos, and practices.
But what is it? The dictionary, quite clinically, refers to abortion as the deliberate termination of a human pregnancy, most often performed during the first 28 weeks. Since time immemorial, women across the world have used a range of traditional home-based practices to terminate unwanted pregnancies for a variety of reasons using whatever techniques, knowledge, and resources they had at hand. Today, the development of modern medicine guarantees women a method of safe abortion that does not jeopardise their health, or put their lives at risk.
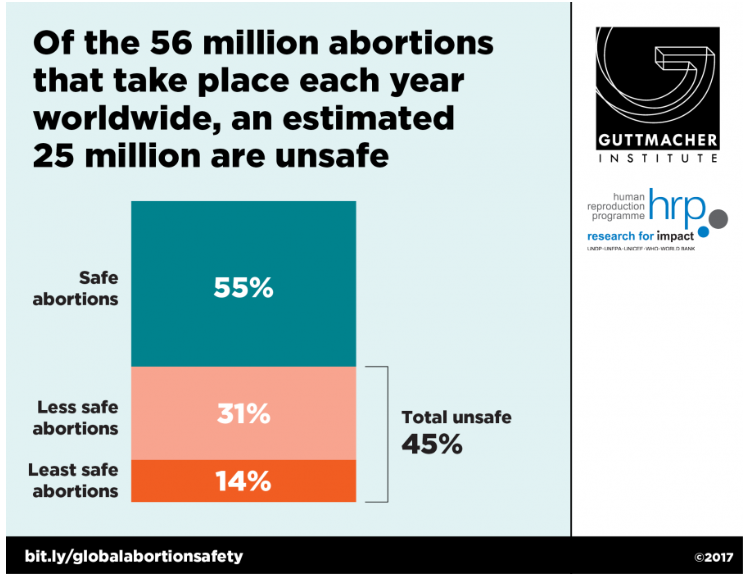
As of 2014, it is estimated that approximately 36 abortions occur each year per 1,000 women aged 15–44 in developing regions, and 27 in developed regions. And yet, the World Health Organisation reports that 45% of all abortions globally are unsafe, which adds up to a staggering number of 25 million unsafe abortions, causing 6.9 million women to be treated for complications arising from unsafe abortions annually. [1]
Much has been said about how ensuring women’s health and rights leads to all-round social gains – economic and otherwise. Indeed, the recognition of this fact is what guided the inclusion of sexual and reproductive health and rights as fundamental to people’s health and survival in the Sustainable Development Goals.
What then prevents women from accessing safe abortion services that are critical to their sexual and reproductive health and wellbeing?
There are a number of explanations that explain women’s inability to access safe abortion services.
One of the main challenges to accessing abortion services is the lack of a legal framework guaranteeing access to abortion services. It is well established that legal abortions are a relatively recent phenomenon with the amendments to criminal codes allowing for abortions only taking place in the mid-to-late 20th century.[2] Indeed, countries like Ireland have only recently won the right to access safe abortion legally, and others like Poland and Argentina continue to fight for the right.
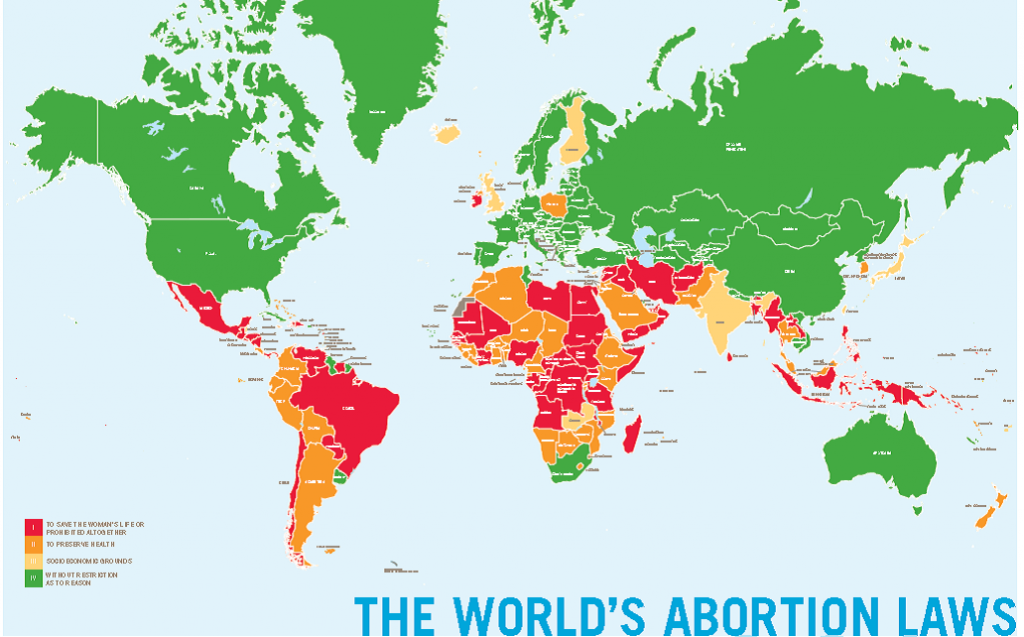
It is necessary to make available both legal and safe abortion services for women; a lack of legal option does not stop women from having abortions, it only necessitates women using unsafe and dubious means of terminating their pregnancies, putting their lives at risk.
The second major challenge to accessing safe abortion services is abortion-related stigma, which cuts across all contexts, continues to negatively affect women’s health and well-being. Accessing safe abortions is strongly influenced by the fear of being recognized by family and friends, the feeling of having done something “wrong”, and of misconceptions about what having an abortion means for future fertility and reproductive health. For as long as such stigma persists, so will unsafe procedures as women avoid trained providers in formal medical settings for the fear of being shamed or judged. [3] Even in countries where abortion is broadly legal, women’s feelings of having a stigmatized procedure can result in their fear of being judged harshly by health professionals, and of being treated as an outcast by their family and community. [4]
A number of other challenges such as cost, availability of trained medical professionals, robust health infrastructure, medical patriarchy all interact to make access to safe abortion close to impossible. Governments, medical associations and civil society organizations must spread the word about any changes in abortion law—most urgently to women, but also medical personnel (including administrative staff) and law-enforcement professionals. Unclear laws and service provision guidelines need to be clarified, especially where abortion continues to be strongly stigmatized. In addition, national health systems must create the required service-provision infrastructure and train personnel, as well as develop, issue, communicate and apply new guidelines.
Only through this can we ensure that women have the ability to exercise control over their own bodies even when institutional provisions exist to guarantee services to women, and no more women’s lives are lost to entirely preventable circumstances.
This blog has only scratched the surface of the debate around access to safe abortion. If you’re keen on learning more, stay tuned to our #AbortionDictionary series as we write about challenges, successes, and issues that relate to the right to safe to abortion.

[1] Singh S., et al. ‘Abortion Worldwide 2017: Uneven Progress and Unequal Access’. 2018. The Guttmacher Institute. https://www.guttmacher.org/report/abortion-worldwide-2017
[2] Henshaw SK, Induced abortion: a world review, 1990, Family Planning Perspectives,1990, 22(2):76–89, http://dx.doi.org/10.2307/2135512.
[3] Astbury-Ward E, Parry O and Carnwell R, Stigma, abortion, and disclosure—findings from a qualitative study, Journal of Sexual Medicine, 2012, 9(12):3137–3147, http://dx.doi.org/10.1111/j.1743-6109.2011.02604.x.
[4] Hanschmidt F et al., Abortion stigma: a systematic review, Perspectives on Sexual and Reproductive Health, 2016, 48(4):169–177, http://dx.doi.org/10.1363/48e8516.